Substrate Preparation
1. On the day of plating, prepare 25 mm coverslips by removing them from 70% ethanol storage solution and propping them up at an angle in each well of a 6-well culture plate to allow drying. [No more than 5 plates (30 coverslips) should be dried simultaneously for 15–25 minutes in culture hood to avoid over-drying.]
2. Once dry, shake slips down flat into their respective wells and coat with 1 mL 0.1% poly-D-lysine, taking care to form a liquid meniscus on each slip. Carefully transfer coverslips into incubator, taking care to preserve meniscus.
3. Incubate for 1 hr at 37°C. [Keeping poly-D-lysine meniscus on top of coverslip is important; this serves to avoid poly-D-lysine coating under coverslip surface that may lead to problematic flotation of coverslip.] After incubation, remove poly-D-lysine and rinse each coverslip three times with 2 mL sterile deionized water. Take care to ensure coverslips do not completely dry at any point during the rinse. After the third and final rinse, leave coverslips in 2 mL sterile deionized water for at least 1 hr. Remove water just before plating, again, make sure to avoid over-drying. [This critical step requires attention. Take care to aspirate off all sterile water remaining from the final rinse, but also use caution as not to over-dry the coverslips. Ultimately, the coverslip must be mostly dry as to allow for the meniscus formation during plating (Fig. 1, Step 12), whereas over-drying can result in the neurons peeling off the glass coverslips days to weeks after plating.]
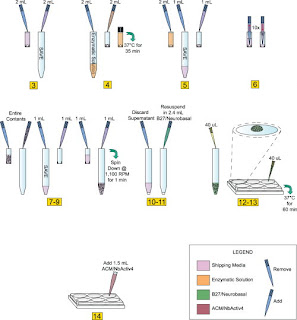
Fig 1: Neuron-Glial Culturing Steps
Preparation of Isolated Neurons (Numbers in Fig. 1 correspond to numbers below).
1. Store tissue at 4°C until ready to use. If dissecting your own cultures, upon isolation of the tissue, store in an appropriate storage media.
2. When ready to plate, make 2 mL of enzymatic solution without B27. In our case, we used Hibernate E-Ca, containing 4 mg (2 mg/mL) of papain. If making your own solution, use a commercially available papain dissociation kit. Make sure to sterile filter solution with 0.2 micron filter after adding papain if source of enzyme is not sterile.
3. Remove the storage media from the dissected tissue and transfer into sterile 15 mL screw-cap tube; be careful not to disturb or remove tissue from original tube. Save the storage media, do not discard.
4. Add 2 mL of media made in Step 2 to tissue (in our case, Hibernate E-Ca containing 2 mg/mL of papain). Incubate for 35 min at 37°C. [Be sure to add Hibernate E-Ca containing papain slowly as to avoid disturbing tissue.]
5. Remove enzymatic solution from tissue, again, take care not to disturb or remove tissue. Add back 1 mL of storage media saved in 15 mL tube.
6. Using a 1 mL pipettor with a sterile plastic pipette tip (tissue can adhere to glass pipettes), aspirate the tissue with the medium into the pipette and immediately dispense contents back into same container. Take care not to create bubbles. [This is another critical step that requires attention. Take care to make sure pipette tip remains in a stable position (as shown in Fig. 1, Step 6). Maintain slow, steady speed when both drawing in and re-dispensing media containing tissue.]
7. Repeat this trituration step 10–12 times or until most all the tissue is dissociated and the cells are dispersed. [Under close examination cell dispersion is highly visible. Stop pipetting immediately upon cell dispersion.]
8. Slowly transfer contents of the tissue tube into a new sterile 15 mL screw-cap tube.
9. Use the remainder of storage medium saved in Step 3 and rinse the interior of the tissue tube before adding it to the sterile 15 mL screw cap tube containing dispersed cells from step 7. [This step helps ensure minimal wastage, as any remaining cells should be saved with this extra rinse.]
10. Spin dispersed cells at 1,100 rpm (200Xg) for 1 min.
11. Discard the supernatant while being careful not to remove any of the cells from cell pellet.
12. Flick tube a few times to loosen the cell pellet. Re-suspend pellet in 2.4 mL of pre-warmed B27/Neurobasal/0.5 mM glutamine medium. Re-suspend by gently pipetting up and down. For E18 Hippocampus, medium includes 25 µM glutamate.
13. Plate cells within a meniscus (approx. 10 mm diameter) at a minimum of 40 µL per 25 mm coverslip. Take care not to disturb meniscus. [Periodically pipette up and down throughout plating process (no more than once every plate per 6 coverslips) to help maintain equal cell density. Again, plating with meniscus formation is critical.]
14. Incubate plated cells at 37°C with 5% CO2 and/or 9% or 20% oxygen for 1 hr.
15. Add 1.5 mL per well of pre-warmed 1:1 ACM/NbActiv4. [Slow and steady media addition rate and proper pipette position are necessary for successful plating density consistency. Position pipette tip at 45° angle along middle of 6-well interior sidewalls, dispense 1.5 mL as slowly and steadily as possible (see Steps 1–14).]
16. Incubate cells at 37°C with 5% CO2 and/or 9% or 20% oxygen.
17. Add Cytosine β-D-arabinofuranoside (Ara-C) to a final concentration of 5 µM, 5–6 days after plating to curb glial proliferation. [Remove 1/3 of media from each well and replace with equal volume containing final concentration of Ara-C]
18. After 4 days or longer, neurons are well differentiated. If further culture is desired, change 1/3 of medium with fresh, pre-warmed 1:1 ACM/NbActiv4 every 7–8 days.
Images: 40X Confocal Images of 30 DIV Hippocampal Cultures. Immunofluorescence detection of MAP-2 (green) and GFAP (red) in 30 DIV (A–C) cultured E18 hippocampal cells using a 40X objective. These images (A and B) clearly depict the intimate physical contact between glia processes and dendritic arbors. Under closer examination (CI and CII), it is clear that the dendrites have grown both bellow (blue arrows) and above (white arrows) glial processes, forming a highly interconnected three-dimensional network by 30 DIV. doi:10.1371/journal.pone.0058996.g004.
All Primary Neuron Assay Customer Publications
- Primary Neurons and Astrocytes-Primary human, rat and mouse neurons and glia/astrocytes.
- Neuronal-Glial Markers-Astrocytes, Glia, Microglia, Olidogodendrocytes, Progenitors and Schwann Cell Markers
- Cells, Cell Culturing Systems and Cell Based Assay Reagents-Cells, Petaka Cell Culturing Systems, Biolumonics Kits, Media, 3-D Scaffolds and Related Reagents Designed to Optimize Cell Based Assays